2021 SNAPSHOT
Highlights of the year

The past year has dealt us a paradoxical mix of highs and lows. After decades of research and investment, the world rejoiced at the World Health Organization’s (WHO) recommendation that the RTS,S/AS01 vaccine should be provided to children living in sub-Saharan Africa to reduce malaria disease and burden. There were also wins in progress towards malaria elimination with news that, despite disruptions due to the COVID-19 pandemic, both China and El Salvador were added to the list of countries to have achieved malaria elimination status.
But it has also been a year of many challenges. We have been faced with some stark numbers – new evidence shows that the COVID-19 pandemic has left a devastating footprint. Beyond the numbers claimed by the virus directly, new data suggests that for every COVID-19 death, more than two women or children have died as a result of disruptions to health systems. Thanks to tireless and outstanding efforts from the global health community, some of the worst-case impact estimates of the pandemic have been averted – such as the projected doubling of deaths from malaria. However, COVID-19 has still significantly exacerbated existing health inequities, diverted critical resources, put vulnerable people further at risk and, according to research from WHO and the World Bank, is likely to halt two decades of global progress towards Universal Health Coverage.
And there are worrying existing and emerging threats beyond COVID-19. Leading scientists and health officials warned at COP26 earlier this year that accelerating climate change threatens unimaginable health consequences. Concern is also growing around a rapidly increasing rise in arboviruses across more than 130 countries, including ones previously unaffected. An estimated 100-400 million people are infected by just dengue alone each year, bringing suffering to mostly young children. Both serve to highlight that we are engaged in a battle in constant flux, influenced by environmental factors, such as climate, human behaviour, and historic interventions. All of which have a knock-on effect on the vectors of these diseases – mosquitoes – that evolve and adapt to counter our efforts.
Malaria Consortium has spent the past twelve months drawing on our strong partnerships first and foremost with communities, and alongside governments, research institutes and other actors in the 15 countries where we have a presence to improve health outcomes and drive progress towards achieving malaria reduction targets, Universal Health Coverage and the Sustainable Development Goals. This is a snapshot of some of the ways we’ve been investing our efforts to have maximum impact.




Large scale disease prevention and burden reduction



Treating 20 million children with anti-malaria drugs
Malaria Consortium teams across Burkina Faso, Chad, Mozambique Nigeria, Togo and Uganda distributed life-saving anti-malaria drugs to around 20 million children.
In countries affected by the highest burden of malaria, large scale operations that achieve high coverage as quickly as possible are critical. Malaria prevention is step one in lowering the cost of malaria to lives and health systems. Seasonal malaria chemoprevention (SMC) involves administering four monthly courses of antimalarial drugs during the period of highest risk, focusing on preventing malaria in some of those who are most vulnerable to the disease - children under five years.
We adapted our programme to ensure it could continue safely in the context of COVID-19 and responded to an urgent call to deliver SMC to two million children in conflict-affected Borno state, Nigeria after a funding gap emerged at late notice.
Delivering seven million LLINs in Nigeria
Thanks to our extensive experience supporting large-scale health campaigns, as well as designing and managing long lasting insecticide treated net (LLIN) campaign evaluation studies, Malaria Consortium has been supporting the mass distribution of over seven million LLINs to help reduce the burden of malaria in Nigeria. The systematic distribution of LLINs, along with information on how to hang, use and maintain them properly, has been at the heart of WHO’s guidance on malaria prevention over the past two decades.
The campaigns are also undertaking household registration, training of local distributors and data collection, as well as extensive monitoring and evaluation research to better understand the cost-effectiveness of LLIN mass distribution campaigns and inform policy and practice of LLIN distribution.
Improving neglected tropical disease (NTD) services in Ethiopia
NTDs affect more than one billion people worldwide, disproportionately impacting the most vulnerable and marginalised communities. Ethiopia has one of the highest NTD burdens in Africa. Supporting the Ethiopian Government to tackle this, Malaria Consortium has been implementing a research study to explore the feasibility, acceptability and cost effectiveness of integrating the prevention, diagnosis, management and reporting interventions of three common NTDs – lymphatic filariasis, schistosomiasis and trachoma – into Ethiopia’s primary healthcare system.
Research that influences policy and practice





This year, Malaria Consortium became one of the only international non-governmental organisations to be awarded Independent Research Organisation status. We are extremely proud that our expertise has been recognised in this way - developing and delivering evidence-based, effective interventions that provide value for money is at the core of our work.
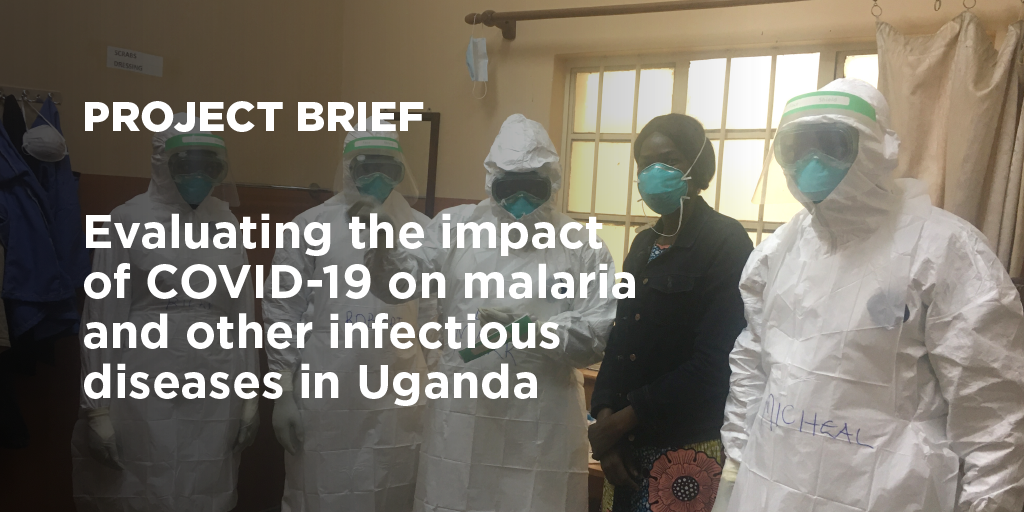
Contributing to critical knowledge of COVID-19 co-infections
We conducted ground-breaking research exploring the potential impact of previous malaria exposure on clinical profiles and outcomes of patients with COVID-19. The results, published in full in The Lancet Microbe found that low previous malaria exposure seems to be associated with more severe manifestations of COVID-19. This preliminary descriptive investigation was the first to characterise potential interactions between SARS-COV-2 infection and malaria and describe important clinical correlates of coinfection in a high burden malaria setting.
Pneumonia research to influence national policy
Pneumonia is the leading cause of death in children under five in both Chad and Ethiopia, accounting for 23 and 16 percent of deaths respectively. We are working with child health partners and the Ministries of Health to develop improved pneumonia control strategies. We’re undertaking a review of the current methods and systems used to manage pneumonia cases at the different levels of the health system and use a consensus approach to develop a Pneumonia Control Strategy (PCS) for each country.
Building the evidence-base for increased malaria prevention for infants in Nigeria
In 2010, WHO recommended intermittent preventive treatment in infants (IPTi), a full therapeutic course of antimalarial medicine delivered to infants through routine immunisation, in areas with moderate to high malaria transmission. However, a decade on, only one country has taken up this recommendation as national policy; Sierra Leone. We're supporting the Nigerian government to research its suitability for uptake within the country and presented early experiences at the American Society of Tropical Medicine and Hygiene Annual Meeting.
Agile responses to emerging challenges



Fragile and conflict settings
As a result of armed violence in Cameroon, many internally displaced persons have insufficient access to basic healthcare, with the closure of over 35 percent of health facilities in the Northwest and Southwest regions. We're helping to improve access to malaria case management for conflict-affected populations in the country.
Find out more about the project
Find out more about the project
Climate
As a leading technical organisation specialising in the prevention, control and treatment of malaria and other communicable diseases, we recognise that climate change has the potential to affect health and disease outcomes for people across the countries in which we work. As a result, we continuously strive to incorporate responses to climate-related risks into our programmes.
Read our position statement on climate
Read our position statement on climate
Resistance
Through the VectorLink project PMI VectorLink: Continuing to Reduce the Burden of Malaria around the World | Abt Associates, We worked with national partners and used an evidence-based approach to develop integrated vector control strategic plans in Malawi and Kenya, and insecticide resistance management plans in Malawi, Kenya, Burkina Faso and Ethiopia. We developed a practical approach to the risk prioritisation and targeting of Insecticide-Treated net distribution campaigns, using several factors including insecticide resistance
Community ownership and leadership



Community health workers key to successful malaria elimination projects
Community health workers are key to delivering health interventions, diagnosing and treating members of their community and engaging them in prevention measures. Despite concern over reduced use of malaria services due to the pandemic, increased service uptake was recorded in provinces in Cambodia where Malaria Consortium is supporting mobile malaria interventions.
Our support to a community-based network of mobile malaria workers has helped to build trust with communities and ensure services are tailored and effective. We believe this model can be replicated in other parts of the world where the continuity of malaria diagnosis and treatment in the community is challenged by pandemics like COVID-19.
Communities leading on behaviour change for better health
We engage community members directly so that their voices and actions help to secure sustainable change. In Ethiopia, we have been promoting social and behaviour change (SBC) interventions to ensure that communities are informed and engaged, supporting the practice of preventive health behaviours and community-led solutions. Through targeted, multi-level SBC approaches, we inform households of the importance of indoor residual spraying of insecticides to combat malaria and encourage them to use LLINs correctly and consistently, seek healthcare early on and adhere to treatments.
Read an overview of the project
Read an overview of the project
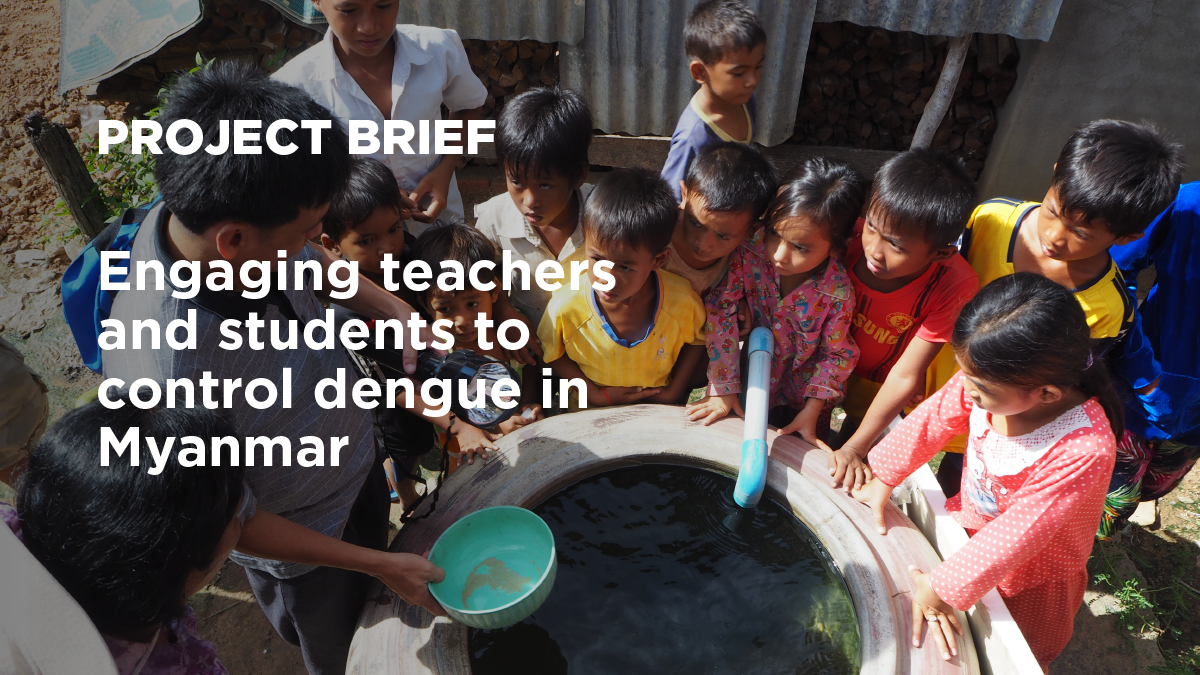
Harnessing the power of young people
Dengue is a priority disease in Myanmar, which has experienced an average of more than 17,000 dengue cases each year since 2010, most of which occur in children under 10. With therapeutic and preventive drugs not yet available — and a vaccine that remains mostly unused due to side-effects — effective vector control is the best way to fight the disease. This requires community involvement and context-specific interventions. Our My School project in Myanmar is assessing the impact of integrated vector control and community-based participatory interventions in schools.
Find out more about the project
Find out more about the project
Strengthening data-informed decision making and digital approaches



Democratising health with digital solutions
Large proportions of the population in low- and middle-income do not have easy or equitable access to healthcare. Digital health platforms, like Malaria Consortium’s upSCALE in Mozambique, are helping to overcome this problem by enabling health workers in local communities to provide diagnosis, treatment and referrals for malaria, as well as logging stock levels of drugs and equipment.
upSCALE enables the Ministry of Health to visualise community data in real time at the district, provincial and national levels of Mozambique’s health system, supporting data-driven decision making around programme investments, surveillance and national health outcomes. The platform was adapted to integrate a diagnostic algorithm for COVID-19 and differential diagnosis for malaria, pneumonia, and diarrhoea, delivering COVID-19 disease messaging and awareness materials via the app and SMS texts.
In 2021, the upSCALE digital platform was introduced in central Uganda to strengthen the existing iCCM programme, The work is currently ongoing and involves capturing community health worker data, assessing if m-Health applications can be used to improve health worker motivation and the inclusion of diagnostic and treatment modules for malaria, pneumonia, diarrhoea and COVID-19.
Hear about upSCALE from health technicians
Strengthening malaria surveillance for data-driven decision making
More effective and integrated surveillance systems will ultimately improve health outcomes and contribute to more resilient health systems that are better able to support public health emergencies like the COVID-19 pandemic. To accelerate malaria elimination, a functional and responsive malaria surveillance system is needed to provide the required intelligence to allocate resources and target interventions effectively. We're supporting the Ministry of Health in Mozambique to design and implement and operationalise an integrated malaria information storage system at district and health facility, strengthen data quality and establish a data-use and data-to-action culture.
Hear from the Director of Mozambique's National Malaria Control Programme, Dr Baltazar Candrinho
Looking ahead
“It is exciting to play a pivotal role in supporting countries to move from ‘undigested’ data overload that has paradoxically resulted in data-driven inertia to efficient decision making, informed by actionable data. This is a key step in building more responsive and resilient health systems, better able to serve communities.”
Arantxa Roca-Feltrer, Head of Surveillance, Monitoring and Evaluation
“What gives me hope for the future is the significant impact of the interventions we deploy, such as seasonal malaria chemoprevention, on reducing the burden of illness and death from malaria. Alongside this, the active involvement the role communities play in utilising and supporting malaria prevention and control activities gives me hope that malaria elimination is really possible.”
Jane Achan, Senior Research Advisor
“I’m very excited about our recently launched projects focused on developing pneumonia control strategies in Chad and Ethiopia, in partnership with the Ministries of Health. Both these countries have some of the highest pneumonia burdens globally and this work will be pivotal in helping to reduce under five morality in both countries.”
Kevin Baker, Research Advisor
“The resilience and dynamism of our staff and in our partnerships to achieve impact, despite the COVID-19 pandemic, has been a humbling experience. I am reinvigorated by our commitment to Universal Health Coverage in our new strategy, and I look forward to working with stakeholders, partners and communities on further progress towards health for all.”
James Tibenderana, Technical Director
“Thanks to the progress we have been making in the 12 years I have been part of Malaria Consortium, for the first time malaria elimination has a place in our strategic intent and I truly believe it is possible to achieve it in the next decade.”
Godfrey Magumba, East and Southern Africa Programmes Director
“I am enormously proud of our ability to reach eligible populations with health interventions even in really challenging operational environments and this reassures me that we are capable in the face of any future challenges. Our work to scale up funding for SMC in Nigeria to cover almost all eligible population despite the economic recession is also extremely encouraging and we plan to apply our learnings to other malaria interventions and make a real contribution to the pathway to Universal Health Coverage. In all of this, we are not forgetting the human element and we will continue to ensure that community voices and actions are amplified and heard.”
Maxwell Kolawole, West and Central Africa Programmes Director